

Melanoma is a malignant tumour of epidermal melanocytes and has metastatic potential. There has been a steady rise in melanoma incidence in fair-skinned populations over recent decades, with the highest figures in Australasia. Primary prevention and early detection are essential, as, despite advances, therapy for advanced and metastatic disease is unsatisfactory. Most melanomas are sporadic and risk factors are genetic and environmental: fair skin, freckles, red hair, number of naevi and sunlight exposure. Thus, patients with multiple atypical naevi (dysplastic naevus syndrome) and fairskinned subjects, often with variant alleles in the melanocortin-1 gene, are at increased risk of melanoma. The type of sunlight exposure is under debate but intermittent exposure, sunburn and sunbed use are implicated. Any family history of melanoma increases individual risk but a strong family history is rare. In familial cases, an autosomal dominant inheritance with incomplete penetrance can occur. Mutations in genes coding for the p16 (CDKN2A) tumour suppressor gene or its binding site are implicated and, in these patients, the lifetime risk of melanoma increases to more than 50%. Advances in molecular technology have identified other susceptibility genes and potential genetic targets for therapeutic intervention in advanced disease.
CLINICAL FEATURES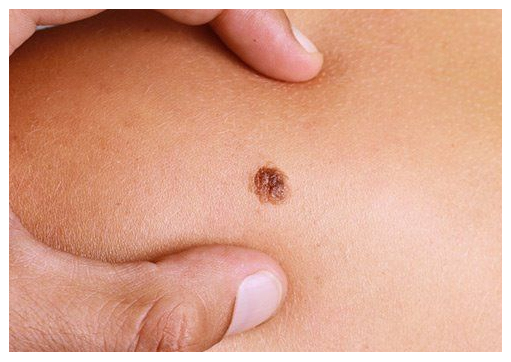
Melanoma can occur at any age and site and in either sex, but typically affects the leg in females and back in males. It is rare before puberty. The classification of invasive malignant melanoma. Early lesions may be in situ and pre-invasive before becoming an invasive SSM. Any change in naevi or development of new lesions should be assessed to exclude malignancy and, for this, the dermatoscope is invaluable. Real-time non-invasive imaging techniques are being investigated as tools to assist in diagnosis but are largely experimental. If in doubt, excision is advised.
SUPERFICIAL SPREADING MELANOMA
Superficial spreading melanoma (SSM) is the most common type in Caucasians. It usually presents as a slowly enlarging, macular, pigmented lesion, with increasing irregularity in shape and pigment; this superficial, radial growth phase can last for approximately 2 years. Subsequently, the lesion becomes palpable and this is indicative of the development of vertical growth phase invasive disease in the dermis; this now has the potential to invade lymphatics and vessels and become metastatic. Approximately 50% of melanomas arise from a pre-existing naevus.
NODULAR MELANOMA
Nodular melanoma is most common in the fifth and sixth decades, particularly in men and on the trunk. This may account in part for the increased mortality rates from melanoma in men, as these are tumours with greater metastatic risk. They often present as a rapidly growing nodule that may bleed and ulcerate. Nodular melanomas may be heavily pigmented, or relatively amelanotic and erythematous, and be confused with benign vascular lesions. A rim of pigmentation may, however, be seen under the dermatoscope. Lesions may develop de novo or from a pre-existing naevus or SSM.
LENTIGO MALIGNA MELANOMA
This is biologically distinct and arises from a prolonged pre-invasive phase, lentigo maligna. It occurs as a very slowly expanding, pigmented, macular lesion, usually on photo-exposed head and neck sites of elderly patients; histology shows in situ changes only. This phase may last for several years before a nodule of invasive melanoma develops in a proportion of cases (lentigo maligna melanoma). Acral lentiginous or palmoplantar melanoma This accounts for only approximately 10% of melanoma in fair-skinned races but is more common in darkskinned people, accounting for 50% of cases and indicating that UVR exposure may not be implicated in acral melanoma risk.
SUBUNGUAL MELANOMA
This form of melanoma is rare. It may present as a painless, proximally expanding streak of pigmentation arising from the nail matrix, and progresses to nail dystrophy and involvement of the adjacent nail fold (Hutchinson’s sign).
HOMOEOPATHIC TREATMENT:
ARSENIC ALB - Cancer arising from overgrowth of fibrous tissues or a cancer originating from the epidermis of the skin- may be hard or soft. Start the treatment with 3c potency and give it four times a day and go on selecting the potency which effects the most. If this remedy cannot cure it will at least reduce the pain and maintain or restore the general health
ARSENICUM IODIDE - Epithelioma. Exfoliation of skin in large scales, leaving a raw exuding surface beneath
ARGENTUM NITRICUM - Melanoma of the skin. Brown, tense and hard skin. Withered and dried up skin. Drawing in skin as from a spider web
CANNABIS SATIVA - Fatty acids present in hemp protect the skin against sun. 15 drops in half a cup of water is used for protection of the skin against the skin cancer due to the sun rays
CONIUM MACULATUM - Epithelioma. Piercing pain, worse at night
EUPHORBIUM — Ulcerating carcinoma and epithelioma of the skin
HYDRSTIS CANADENSIS- Cancerous formation of the skin. Skin is ulcerated with small pox like eruptions
KALI ARSENIC- Skin cancer with no other visible symptoms except many small nodules under the skin
LOBELIA ERNUS- Epithelioma , that is malignant tumor consisting principally of epithelial cells originating from the epidermis of the skin or in a mucous membrane and developing rapidly . Dryness of the skin, nose and mucous membrane of the cheeks
LYCOPODIUM CLAVATUM 200- Skin hard and indurated. Epithelioma. Visicid and offensive perspiration
RADIUM BROMIDE 30- Cancer of the skin with itching, burning and restlessness.